Fragile X syndrome: What do we know about it and how do we promote a child’s participation and independence?

What is Fragile X syndrome?
Fragile X syndrome (FXS) is a genetic disorder that affects a specific gene on the X-chromosome. This gene is called the fragile X mental retardation 1-gene or FMR-1 gene, which is found in every cell of the body (Hagerman et al., 2017). The protein made by the gene is essential for normal brain development. In the case of Fragile-X syndrome, it either does not make this protein or makes too little of it. Therefore, the brain does not develop normally.
Prevalence and comorbidities
Fragile X syndrome is the leading cause of inherited intellectual disability worldwide and the second-most common cause of intellectual disability after Down syndrome (Dykens & Hodapp, Robert M. and Finucane, 2000). The exact number of people who have Fragile X syndrome is unknown. However, a review of research studies estimated that about 1 in 7,000 males and about 1 in 11,000 females have been diagnosed with Fragile X syndrome (Hunter et al., 2014). They show comorbidities with other disorders such as attention deficit hyperactive disorder (ADHD), autism spectrum disorder (ASD), and anxiety (Mckechanie et al., 2019). ADHD estimates of comorbidity have been established at 73% (Baumgardner et al., 1995). However, recent studies have stated a prevalence of comorbid Fragile-X syndrome and ASD that varies from 23 % to 67% (Dykens & Hodapp, Robert M. and Finucane, 2000), however, the presentation often varies subtly from that seen in classic ASDs.
Clinical presentation
Clinical presentation may differ from one child to another, however, common signs can be observed, where symptoms are often milder in females than in males (Mckechanie et al., 2019). Clinical features and manifestation differ by age (Hagerman et al., 2017) and can be divided into four categories (Bailey et al., 2009; Lubala et al., 2018):
- Physical features: Except for the joint hypermobility noticed in infants and children, most of the physical features are developed during the puberty period such as a narrow face, large head, large ears, flat feet, and a prominent forehead.
- Developmental delay: Problems with intellectual functioning and cognitive skills are commonly encountered in children with Fragile X syndrome . Intellectual problems can range from the mild, such as learning difficulties or problems with mathematics, to the severe, such as an intellectual or developmental disability, that might affect specifically the independence in daily life activities. Furthermore, it has been reported that Intellectual level contributes to impaired motor abilities of children diagnosed with Fragile X syndrome (Zingerevich et al., 2009). Language delay is observed less frequently than the developmental delay. It affects boys more than girls. While few children are non-verbal, most of them can talk. They might show difficulties in speaking clearly.
- Social and emotional issues: Children with Fragile X syndrome often show behavioral challenges. They may show anxiety and fears in new situations, as well as hyperarousal manifestations They may have difficulties in making eye contact with other people. Attention disorders and hyperactivity can also be encountered.
- Sensory issues: Many children with Fragile X syndrome are bothered by certain sensations, such as bright light, loud noises, or the way certain clothing feels on their bodies. These sensory issues might cause them to act out or display other behavioral problems. Major sensory issues can also affect gross motor and fine skills such as balance abilities, jumping or running as well as manipulating objects.
Diagnosis
At birth, infants with Fragile X syndrome often exhibit no clinical signs, with most parameters (e.g., head circumference, weight, and height) in the normal range (William L. Stone; Hajira Basit; Evan Los., 2022). According to a national parent survey sponsored by the Centers for Disease Control and Prevention (CDC) (Bailey et al., 2009), it has been noticed that parents are first report their concerns when the child is 12-month-old, often reporting a hypotonia followed by a developmental delay around the crawling and walking age. While the average age of a developmental delay confirmation by professionals is at the age of 20 months, the Fragile X syndrome diagnosis is not defined until the age of 36 months (Bailey et al., 2009).
It was not until 1992 that a test genetics to diagnose the syndrome has been developed: it consists of analyzing the repeated sequence near the FMR1 gene; it is carried out on a simple blood sample, collected by a blood test. The genetic test does not allow to evaluate the severity of the disease. Additional information based on occupational, speech and language, and psychological evaluation are necessary to best adapt the rehabilitation and pedagogical program to the child’s specific skills and difficulties.
How to support the participation and independence in children with Fragile-X Syndrome
Although there is no empirically validated occupational therapy intervention for children with Fragile X syndrome, the evidence-based intervention in autism and other developmental disabilities should be applied (Grace T Baranek, 2002). Treatment strategies in occupational therapy, which promote independence in daily life activities are based on the following:
- Sensory integration therapy:
Hyperarousal is probably the most challenging aspect of Fragile X syndrome (Reiss & Hall, 2007). Hyperarousal is an intense feeling of anxiety, and nervousness, which can be manifested with behavior like aggression, self-harm, high levels of impulsivity.
Hyperarousal impacts everything—as hyperarousal goes up, skill levels go down a bit like a seesaw.
Physiological symptoms of Hyperarousal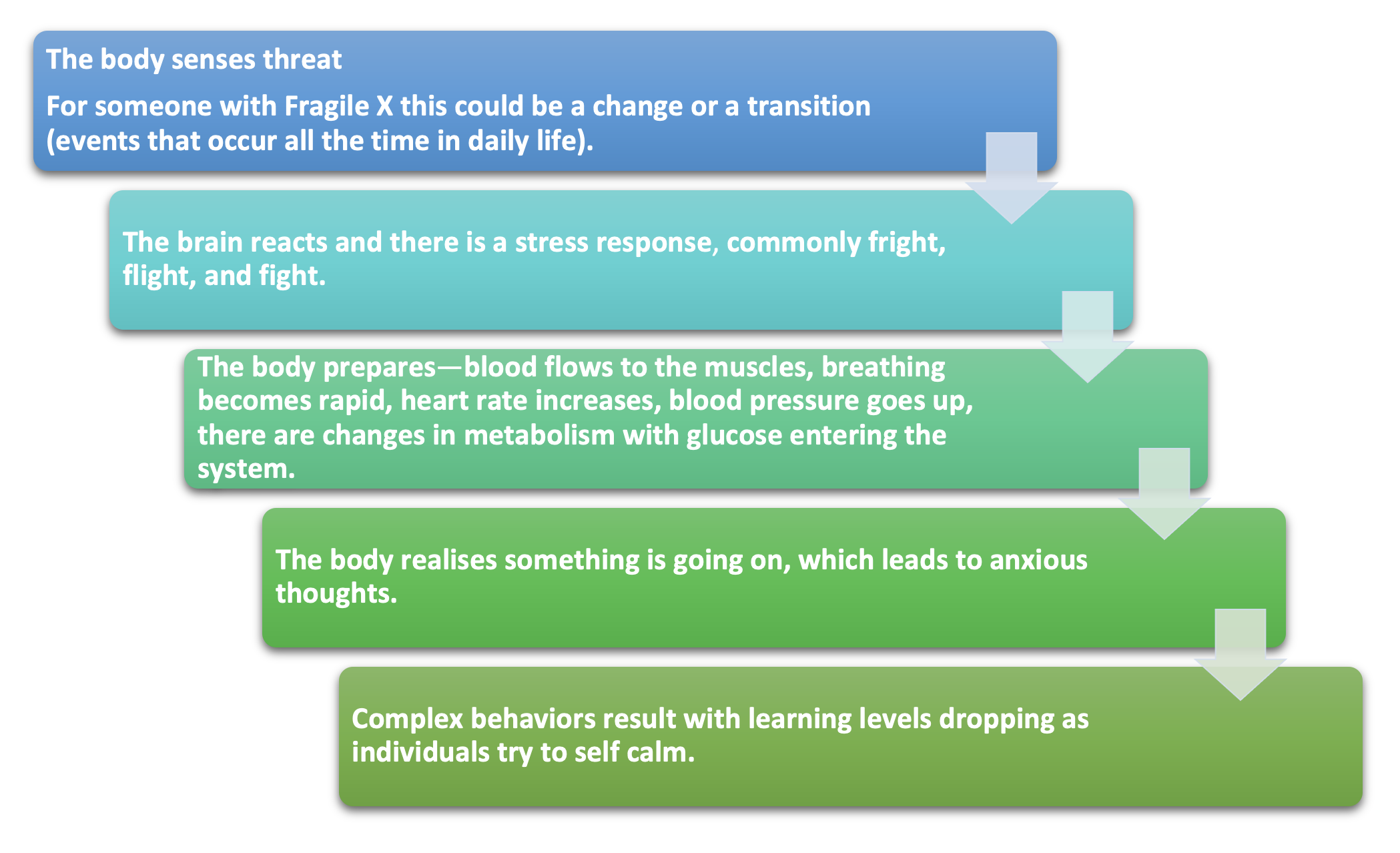
Managing hyperarousal in individuals with Fragile X syndrome is key to helping them to participate successfully in their everyday life and reach their maximum potential across the different life settings.
This is because hyperarousal is a disorganized state, leading to temporarily compromised language, social and motor skills, and sometimes challenging behaviors (Malden, 2004) .How can hyperarousal be managed?
-
Sensory-based strategies:
The sensory diet is often adopted to address hyperarousal. It is based on making sure that sensory strategies are routinely embedded during the day to help the person with Fragile X syndrome to be self-regulated and prevent hyperarousal state during the day. The sensory diet includes different components:- Deep pressure activities like a massage.
- Strenuous physical activities to calm down the system, such as lifting, pulling, and pushing. Sometimes yoga-style activities can be helpful, such as pushing a ball.
- Fidget toys can help to keep an individual in just the right state.
- Movement-based activities such as swinging, rocking, dancing, or horseback riding.
- Sensory box , which contains things the child enjoys using, like something to suck, fidget toys as mentioned above, matching games, and simple puzzles.
Only certified professionals, such as High Hopes’ occupational therapists, are trained to deliver sensory integration therapy and the sensory diet.
- Routine-based strategies:
Individuals with fragile X syndrome can be stressed by transitions whilst liking routines. Considering this, it is important to keep things as predictable as possible with routine-based strategies. This includes the use of visually structured routines throughout the day, including visual schedules and the use of visual strategies for specific skill development (Rodger and J. Ziviani, 2006).
-
Sensory-based strategies:
- Developing abilities:
The occupational therapy intervention aims to develop a broad range of skill areas to foster independence in daily life activities such as hygiene, cleaning, cooking, money handling, and domestic duties.Occupational therapist uses different approaches to support skills development, such as:
- Providing alternative ways to reach independence in a specific task, for example clothing styles with few or no closures, or simpler closures that feature using larger buttons, hooks, or Velcro straps.
- Incorporating cognitive planning and problem-solving strategies to teach skills in a step-by-step manner.
- Social skills training:
Occupational therapist uses skills training and social stories to:- Develop self-care skills (for example, how to clean teeth, wash hands or get dressed), social skills (for example, sharing, asking for help, saying thank you, interrupting) and academic abilities (Reiss & Hall, 2007).
- Help the child understand how others might behave or respond in a particular situation.
-
Gross and fine motor skills Development:
Occupational therapists work on developing the underlying skills necessary to support whole body (gross motor) and hand dexterity (fine motor) skills, such as providing activities to support:- balance and coordination;
- strength and endurance;
- attention and alertness;
- body awareness; and,
- movement planning.
- School transition: Advocating and professionally supporting the transition to school and liaising with teachers as required.
- Devise goals: Setting functional and achievable goals in collaboration with the child, parents, caregivers, and teachers so that therapy has a common focus beneficial to everyone involved.
- Educating: Parents, caregivers, teachers, and others involved in the child’s care about Fragile X syndrome and the age-appropriate skills a child should be demonstrating to be self-regulated and prevent hyperarousal state during the day.
For more information about supporting your child and to understand more about Fragile-X syndrome, please speak to one of High Hopes’ occupational therapists. They will work on implementing an individual treatment plan within a holistic approach while collaborating with other therapists such as speech and language therapists, psychologists, or others if necessary.
Sources:
- Bailey, D. B., Raspa, M., Bishop, E., & Holiday, D. (2009). No change in the age of diagnosis for fragile X syndrome: Findings from a national parent survey. Pediatrics, 124(2), 527–533. https://doi.org/10.1542/peds.2008-2992
- Baumgardner, T. L., LReiss, A., Freund, L. S., & Abrams, M. T. (1995). Specification of the neurobehavioral phenotype in males with fragile X syndrome. Pediatrics, 5(May), 744–745.
- Dykens, E. M. ., & Hodapp, Robert M. and Finucane, B. M. (2000). Genetics and mental retardation syndromes: A new look at behavior and interventions. (M. P. H. B. Baltimore (ed.)).
- Grace T Baranek. (2002). Efficacy of Sensory and Motor Interventions for Children with Autism. Journal of Autism and Developmental Disorders, 32(5), 397–422. https://doi.org/10.1023/A:1020541906063
- Hagerman, R. J., Berry-Kravis, E., Hazlett, H. C., Bailey, D. B., Moine, H., Kooy, R. F., Tassone, F., Gantois, I., Sonenberg, N., Mandel, J. L., & Hagerman, P. J. (2017). Fragile X syndrome. Nature Reviews. Disease Primers, 3, 17065. https://doi.org/10.1038/nrdp.2017.65
- Hunter, J., Rivero-Arias, O., Angelov, A., Kim, E., Fotheringham, I., & Leal, J. (2014). Epidemiology of fragile X syndrome: A systematic review and meta-analysis. American Journal of Medical Genetics, Part A, 164(7), 1648–1658. https://doi.org/10.1002/ajmg.a.36511
- Lubala, T. K., Lumaka, A., Kanteng, G., Mutesa, L., Mukuku, O., Wembonyama, S., Hagerman, R., Luboya, O. N., & Lukusa Tshilobo, P. (2018). Fragile X checklists: A meta-analysis and development of a simplified universal clinical checklist. Molecular Genetics and Genomic Medicine, 6(4), 526–532. https://doi.org/10.1002/mgg3.398
- Malden, M. (2004). Sensory integration. Paper Delivered as Part of a One-Day Seminar on Fragile X Syndrome for the Fragile X Resource Group of Greater Chicago on 23 Oct. 2004, 303 p.
- Mckechanie, A. G., Barnicoat, A., Trender-gerhard, I., Allison, M., & Stanfield, A. C. (2019). Clinical Intelligence Fragile X-associated conditions: HOW ARE INDIVIDUALS WITH FRAGILE X. British Journal of General Practice, 69(September), 460–461.
- Reiss, A. L., & Hall, S. S. (2007). Fragile X Syndrome: Assessment and Treatment Implications. Child and Adolescent Psychiatric Clinics of North America, 16(3), 663–675. https://doi.org/10.1016/j.chc.2007.03.001
- Rodger and J. Ziviani. (2006). Occupational Therapy with Children: Understanding Children’s Occupations and Enabling Participation. In Occupational Therapy In Health Care (Vol. 22, Issue 4). https://doi.org/10.1080/07380570802244605
- William L. Stone; Hajira Basit; Evan Los. (2022). Fragile X syndrome. In STATEPEARLS. StatPearls Publishing.
- Zingerevich, C., Greiss-Hess, L., Lemons-Chitwood, K., Harris, S. W., Hessl, D., Cook, K., & Hagerman, R. J. (2009). Motor abilities of children diagnosed with fragile X syndrome with and without autism. J Intellect Disabil Res, 53(1), 11–18. https://doi.org/doi: 10.1111/j.1365-2788.2008.01107.x. Epub 2008 Sep 3.